Insurance Coverage for RestoreX and RestoreXL
Get Reimbursed for Your Penile Traction Device
Many insurance plans may cover the cost of RestoreX and RestoreXL. Follow these simple steps for your specific insurance type below to submit a claim.
RestoreX and RestoreXL are FDA-registered medical devices prescribed by physicians.
RestoreX and RestoreXL have a dedicated, permanent billing code (HCPCS E0740).
Choose Your Insurance Type
Start My Private Insurance Claim
Option 1: Private Insurance (e.g., Aetna, Blue Cross, Cigna, United Healthcare)
Private Insurance (e.g., Aetna, Blue Cross, Cigna, United Healthcare)
A simple, 3-step process to submit a claim to your private insurance provider.
Step 1: Purchase your device:
- Purchase the device directly from RestoreX.com
- Print your PathRight Medical purchase receipt.
Step 2: Get a doctor’s prescription:
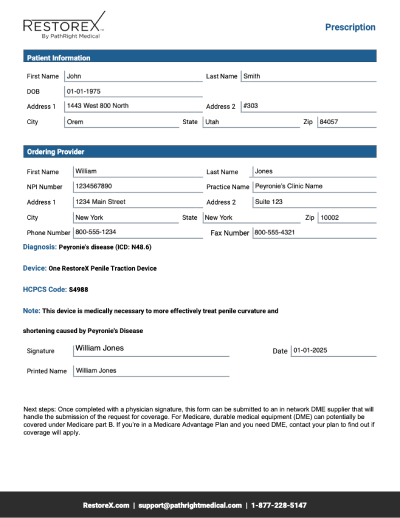
- Download the prescription form PDF.
- Your doctor must write a prescription specifying the exact device you need, including the type, quantity, and reason for medical necessity. You can use our prescription form to facilitate this.
- Although a prescription is not required to obtain the RestoreX or RestoreXL device, it may facilitate receiving reimbursement from your insurance provider.
Step 3: Submit your claim:
- Submit both documents to your insurance provider:
- The signed prescription PDF.
- Your PathRight Medical purchase receipt.
- The signed prescription PDF.
- Supporting Info: You can find the claim submission process on your insurer’s website or by calling your member services number.
Option 2: Medicare
Step 1: Download our prescription form for RestoreX and RestoreXL
- Your doctor must write a prescription specifying the exact DME you need, including the type, quantity, and reason for medical necessity. You can use our prescription form to facilitate this.
- Locate a DME supplier that is in your insurance network and can bill your private insurance for the equipment.
- For a Medicare DME supplier directory, you can search here: https://www.medicare.gov/medical-equipment-suppliers/
Or find a DME supplier in network with your private insurance company
- Some private insurance companies, like Aetna, have provider directories that you can use to search for in-network suppliers.
- To search for a directory like this for your insurance, simply google “(name of your insurance) DME supplier search” or other search variations.
- Give your doctor’s prescription to the DME supplier.
- The DME supplier will submit the claim to your insurance on your behalf, including the prescription and any necessary supporting documentation.
- Prior authorization: Some DME items might require prior authorization from your insurance company, which means your doctor needs to get approval before the equipment can be dispensed.
- Coverage verification: Always confirm with your insurance company what type of DME is covered and what specific requirements they have for submitting a claim.
- In-network providers: Using a DME supplier that is in your insurance network can help minimize out-of-pocket costs.
Frequently Asked Questions (FAQ)
What is the HCPCS code for RestoreX/RestoreXL?
The permanent billing code is E0201, described as a “penile stretching device.” This code can be used for private insurance submissions.
Will my insurance definitely cover RestoreX/RestoreXL?
Coverage decisions are made by individual insurance providers. We cannot guarantee reimbursement, but providing a signed letter of medical necessity significantly improves your chances. If your provider is in-network with your insurance, it is also more likely that they will cover the device.
Why do I have to purchase the device first for private insurance?
This direct-to-patient model simplifies the process. Submitting a claim with a receipt for a purchased device is the most common path for reimbursement for medical devices of this type.
It is possible for your physician to submit the claim on your behalf, however, most offices will not be set up to do this. It is also not more or less likely that your claim will be approved depending on who submits the claim.
What if my private insurance claim is denied?
If your claim is denied, you have the right to appeal the decision. Contact your insurance provider for details on their appeals process. Your clinician’s office may be able to assist you.
Including a custom letter of medical necessity will likely increase your chances of achieving a successful appeal.
PathRight Medical was formed in 2015 to meaningfully improve the lives of men with Peyronie’s disease or those with side effects associated with urological surgeries or chronic disease. PathRight Medical developed RestoreX in cooperation with Mayo Clinic.

Contact us
PathRight Medical, Inc.
1443 W 800 N
Suite 303
Orem, UT 84057
CALL: 1-877-228-5147